
Gluteus Medius Tendinopathy: What You Need to Know
What is the Gluteus Medius?
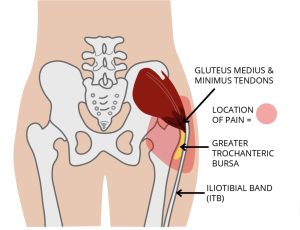
The gluteus medius is one of your main hip stabilising muscles. It sits on the outside of your pelvis and attaches to the top of your thigh bone (femur). Every time you walk, run, or balance on one leg, your gluteus medius works to keep your hips level and your pelvis stable.
When the tendon that attaches this muscle to the bone becomes irritated or overloaded, it’s called gluteus medius tendinopathy (sometimes also called “lateral hip tendinopathy” or part of Greater Trochanteric Pain Syndrome).
Common Symptoms
Gluteus medius tendinopathy usually feels like:
- Pain on the outside of the hip (around the bony bump at the top of your thigh)
- Pain worse with walking, running, climbing stairs, or standing on one leg
- Difficulty lying on the painful side at night
- Stiffness or weakness when you first get up after sitting
It can start gradually, often without one clear injury, and can become very limiting if left untreated.
Causes and Risk Factors
Gluteus medius tendinopathy is usually due to overload, poor mechanics, or age-related changes in the tendon. Common causes include:
- A sudden increase in walking, running, or stair climbing
- Weak gluteal and core muscles, leading to more strain on the tendon
- Poor movement patterns (hip drop, knees caving in)
- Hormonal changes (more common in women around mid-life)
- Previous back or hip problems that alter your gait
Diagnosis
A physio can usually diagnose gluteus medius tendinopathy by listening to your history and testing specific movements (e.g., standing on one leg, resisted hip abduction).
Scans like ultrasound or MRI can show tendon irritation, but they’re not always needed — and often don’t change the best treatment approach.
What Actually Helps?
Good news: gluteus medius tendinopathy responds really well to physiotherapy. The key is reducing aggravating positions and gradually strengthening the hip.
Evidence-based treatment includes:
- Load management: avoiding lying on the painful side, and limiting long walks/runs that flare it up
- Hip and glute strengthening: exercises like Isometric Hip Abduction (with Loop Band around knees), Bridges, band walks, and carefully progressed functional strengthening exercises.
- Movement retraining: teaching your body to keep the pelvis stable when you walk or climb stairs
- Manual therapy: hands-on treatment for pain relief in the early stages
- Education: knowing which positions and postures help vs. worsen your hip pain
Steroid injections are sometimes used, but research shows that in the long run, exercise-based rehab gives better results.
When to Seek Help
If your hip pain is stopping you from sleeping, walking, or exercising the way you want, don’t wait for it to “go away on its own”. Early, tailored rehab makes recovery much faster — and prevents it becoming a long-term issue.
Takeaway
Gluteus medius tendinopathy is one of the most common causes of outer hip pain, but with the right guidance and exercise program, most people recover well.
At LivFit Physio Mornington, we’ll assess your movement, identify the cause of your pain, and build a personalised program to get you back to doing what you love.
👉 Book your initial consultation today and start your recovery.